- By - Malfaifi
- Posted on
- Posted in Implant Dentistry
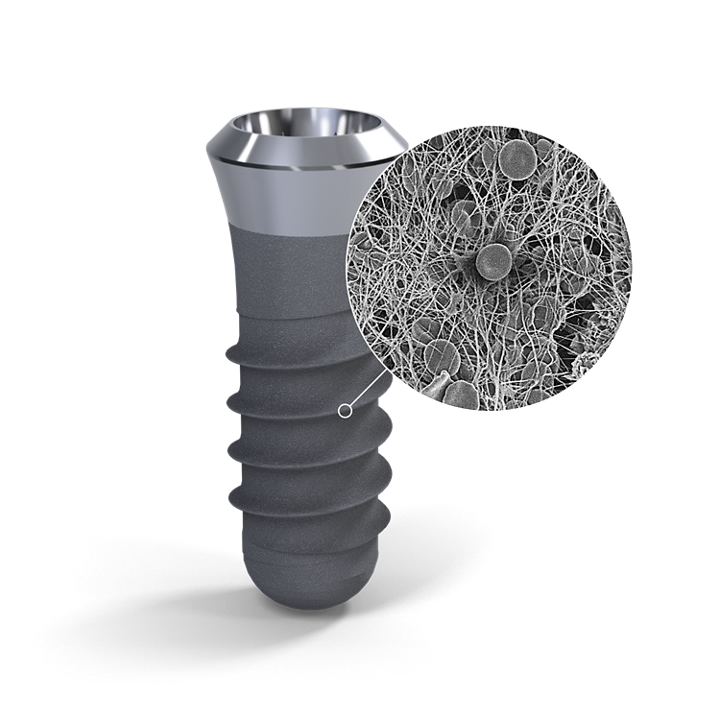
Topographic Implant Surface
Oral Implant Surfaces: Part 1—Review Focusing on Topographic and Chemical Properties of Different Surfaces and In Vivo Responses to them
Albrektsson et al 2004
Morra et al found that machined implants display a lower concentration of titanium on the surface and a higher concentration of carbon than sandblasted, acid- etched, or plasma-sprayed surfaces.
Wear is related to the strength of the material, but also to surface roughness.
Implants of a roughness of about 1.5 µm (Sa) show stronger bone response than turned (smoother) and plasma-sprayed (rougher).
Potential drawbacks of roughening the implant surface include greater problems with Peri-implantitis and a greater risk of ionic leakage.
1.0–2.0 µm (“moderately rough”) Tioblast, SLA, TiUnite, Frialit, most implants of today.
Stronger bone response, tendency to better clinical results than turned implants Many, but not all, designs have only short clinical follow-up _ 2.0 µm (“rough”) Plasma-sprayed titanium, hydroxyapatite-coated implants Positive 5-year documentation reported
Increased incidence of Peri-implantitis reported in two studies.
The relevant way to describe an oral implant surface is by referring to its micrometer-sized irregularities.
Physical characteristics refer to factors such as surface energy and charge.
In other words, an oral implant with high surface energy may, at least theoretically, show stronger ossseointegration than implants with a low surface energy.
It is possible that an initially high surface energy will be immediately changed when the implant is moved from the glow discharge container through the air toward the patient.
A turned titanium implant, such as the original Brånemark screw, is anchored to bone through in- growth into small irregularities of the implant surface— biomechanical bonding.
Scientific papers published into the 1980s generally indicated that bone needs a minimum of 50- to 100-µm cavities or pores for proper ingrowth.
Today, we have sufficient knowledge that irregularities at least down to 1 µm may be invaded by bone, although complete Haversian systems need a larger space.
The strongest biomechanical bonds are seen to surfaces of a roughness of about 1.5 µm, whereas rougher, plasma-sprayed implants show weaker bone ingrowth.
Biochemical Bonding
The best definition of the biochemical bonding mode of implant anchorage is: “Bioactivity is the characteristic of an implant material which allows it to form a bond with living tissues.”
Potential chemical bonding between implant and host tissues was first suggested by Hench et al and referred then to a certain glass-ceramic composition and its reaction to the host tissues.
Instead, calcium phosphate ceramics (eg, hydroxyapatite [HA]) were launched as potentially bioactive surface coatings for titanium implants.
Calcium phosphate–coated implants.
As summarized by Legeros, calcium phosphate biomaterials have similarities to bone mineral: They may form bone apatite like mineral or carbonate HA on their surfaces (bioactivity); they are able to promote cellular function, leading to formation of a strong bone–calcium phosphate interface; and they are osteoconductive and may bind bone morphogenetic proteins (BMP) to become osteoinductive.
Osseotite acid- etched implants (3i) have been claimed to give rise to a particular fibrin retention that allows osteogenic cells to migrate to the implant surface, enabling what Davies 53calls “de novo bone formation.”
Doped Surfaces
Under this heading are implant surfaces that have been doped with a potentially bone-stimulating agent, such as BMP or other bone growth factors.