- By - Malfaifi
- Posted on
- Posted in Uncategorized
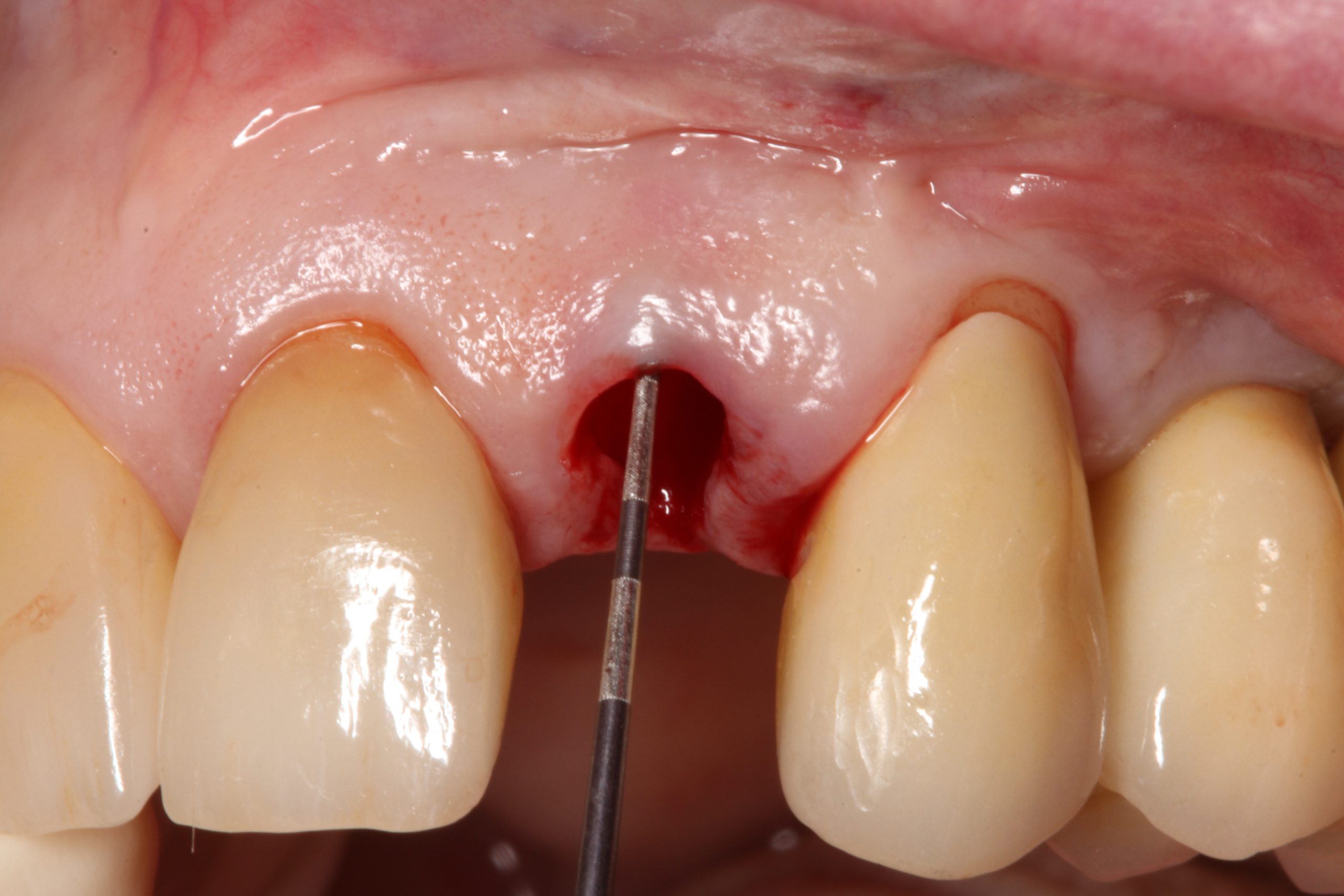
Peri-implant soft tissue phenotype modification
Peri-implant soft tissue phenotype modification and its impact on peri-implant health: A systematic review and network meta-analysis
Tavelli et al 2020

A review on clinical studies that involved soft tissue augmentation around dental implants and reported findings on KMW, MT, and/or STH changes.
- Insufficient amount of keratinized mucosa width (KMW) < 2mm around dental implants is associated with more plaque accumulation, tissue inflammation, mucosal recession, and/or attachment loss probability of developing marginal bone loss.
- Mucosal thickness can also provide greater stability of the mucosal margin which prevent mucosal recession. As well as promote greater stability of interproximal marginal bone levels.
- Insufficient of supracrustal tissue height (STH), is associated with greater marginal bone loss (MBL) particularly when the implants placed at the level of the bone crest.
- Different techniques to increase the peri-implant soft tissue phenotype (PSP), which includes KMW, MT, and STH, like autogenous soft tissue grafts (either the free gingival graft (FGG) or connective tissue graft (CTG)
Summary of the results:
- Significant increase in KMW when soft tissue grafts particularly FGG were used in combination with Apical positioned flap (APF). This approach resulted in reductions in probing depth, peri-implant soft tissue dehiscence, and plaque index.
- CTG has been generally recommended as the grafting material of choice when treating peri-implant soft tissue dehiscence.
- Implants placed in sites presenting thin supracrestal tissue height (STH) are associated with increased marginal bone loss compared to implants placed in the presence of naturally thick STH or STH that was augmented at the time of implant placement.
- Bilaminar techniques in combination with connective tissue graft or acellular dermal matrix were superior to Collagen matrix in terms of mucosal thickness gain.