- By - Malfaifi
- Posted on
- Posted in Implant Dentistry
Guided bone regeneration
Guided bone regeneration at oral implant sites
Hämmerle et al 1998
This paper discusses the scientific and clinical aspects of guided bone regeneration (GBR).
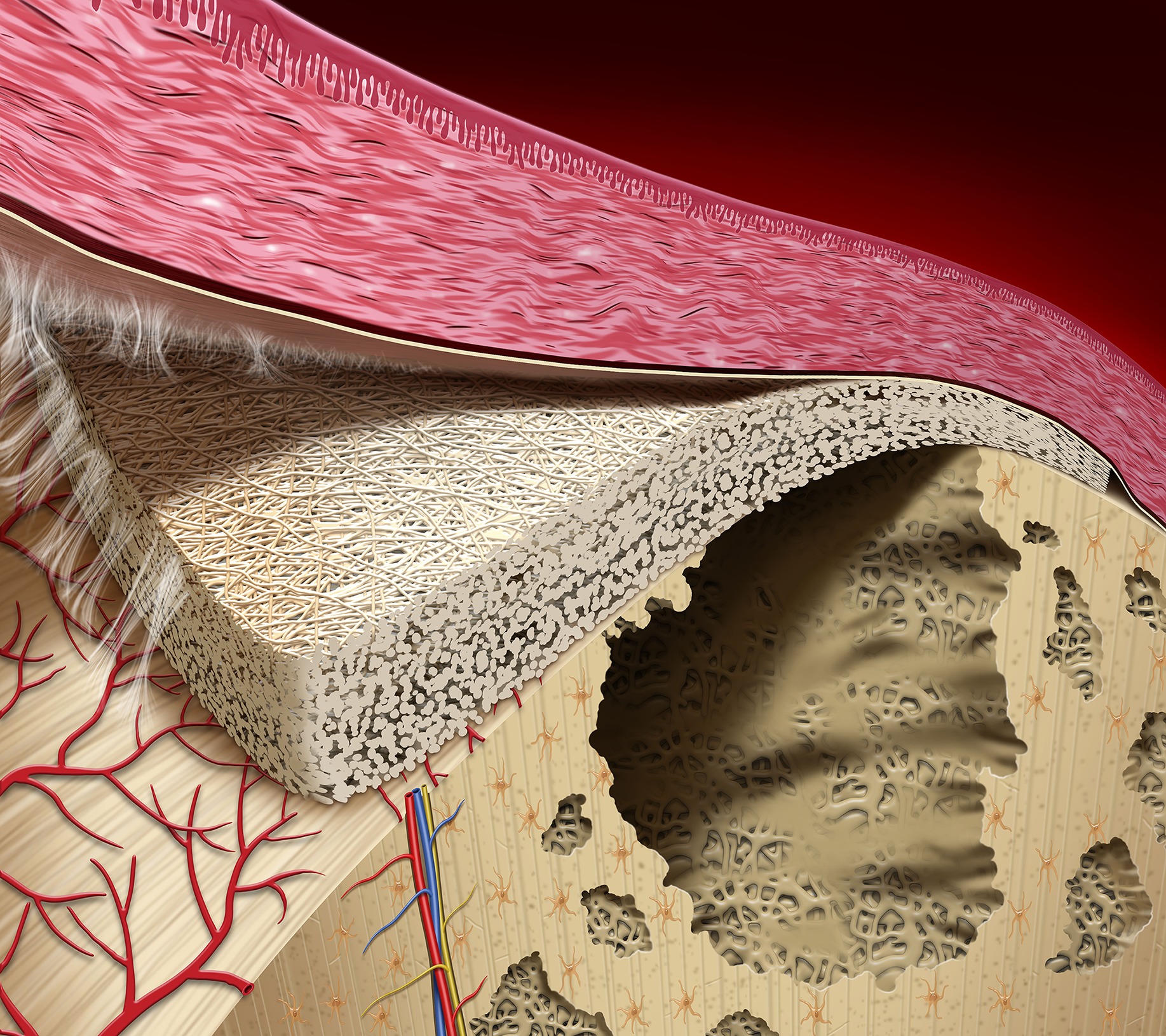
GBR uses the principles of guided tissue regeneration (GTR), the separation of soft tissue from bone by barrier membranes, to generate bone.
Nyman and Karring (early 1980s) developed the method of GTR.
Four methods to augment bone volume:
1) osteoinduction – growth factors,
2) osteoconduction – scaffold material,
3) distraction osteogenesis – fracture created and slowly pulled apart,
4) GTR – spaces maintained by barrier membranes.
GBR has shown the best and most predictable results to fill peri-implant bone deficits.
Problems with GBR:
1) collapse of barrier membrane,
2) exposure of membrane → local infection, incomplete bone regeneration.
During GBR, new woven bone is formed in the space provided by membrane.
This is eventually remodeled into mature lamellar bone.
Applications of GBR:
1) GBR prior to implant placement
Indications;
- Bone deficit at a site where primary stability of an implant cannot be achieved, implant placement not possible in ideal location for pros tx.
- Lateral ridge augmentation has been shown to be more predictable than vertical augmentation.
Investigations show that regenerated bone is capable of withstanding occlusal loading forces transmitted by implant prosthesis and this bone is stable over time.
2) GBR in conjunction with implant placement.
The one-stage method of combining implant placement with GBR has been applied much more frequently than the two-stage method using GBR prior to implant placement.
Membrane exposures and localized infections can compromise results.
The newly formed bone has been shown to osseointegrate with the exposed surface.
In situations with extensive bone defects following tooth extraction, the two-stage approach is generally preferred.
Disadvantage; if GBR is compromised, only the more apical part of the implant will be properly osseointegrated.
3) GBR at transmucosal implants.
Flap is adapted around the neck of the implant, covering the membrane but leaving the implant in a transmucosal position.
Infection control seems to be more important for optimal tx outcome than whether implant is submerged or transmucosal.
4) GBR in the treatment of peri-implant defects.
It is of paramount importance to realize that the infectious disease process has to be adequately treated prior to regenerative surgery.
Rationale for use with GBR; support for the membrane, provides scaffold for ingrowth of capillaries and perivascular tissue (osteoprogenitor cells), a carrier for growth factors.
Bone inductive materials. Growth factors, found in DFDBA. Autogenic bone.
Integration of natural bone mineral has been shown to be superior to coral- or algae-derived HA.
Bovine-derived bone mineral exhibiting natural crystallinity (Bio-Oss) yielded increased bone-to-graft contact compared with a product of the same origin but with larger crystal size (Endobon).
Calcium phosphate compounds as well as coral or algae-derived materials degrade over time.
Conflicting results have been published regarding the long-term performance of natural bone mineral.
Currently developing resorbable grafting materials based on synthetic polymers. These can be used as carriers for growth factors.
Resorbable membranes.
Advantage; eliminates retrieval surgery.
Resorbable membranes need a bone graft to maintain space.
They can be used successfully for GBR around implants.
To expand your knowledge on this topic read
Courtesy of Wilford Hall Medical Center-USAF Prosthodontic Residency